by Lucinda Staniland
I used to think that alignment and biomechanics were the answer to the riddle that is chronic pain. If only I could work hard enough to correct my hyperlordosis, strengthen my weak glutes, and reverse my scoliosis then my pain would ease – right? At least, that’s what I was told.
Now, I’m not so sure.
In fact, I’ve found that I’ve been able to reduce my chronic pain significantly without changing my biomechanics or alignment at all. In fact, I now wonder if my focus on these factors was actually making my pain worse.
Although yoga is a holistic practice, I’ve found that when it comes to pain, many yoga teachers focus almost exclusively on biomechanics and alignment.
At first, this seemed intuitive to me. I have pain, I thought, so I need to fix the damaged tissues that are causing pain, and then also fix the structural imbalances that are damaging my tissues.
But when I started researching pain science, I realised that, strangely, this isn’t actually how pain works. At least, not chronic pain, which is defined as pain that lasts more than 3 months. In chronic pain, tissue damage is just one factor that can cause pain. And, sometimes, it may not be the most important one.
In fact, research regularly finds that asymptomatic populations – a.k.a those fortunate pain-free people – often have significant tissue damage, such as herniated discs, torn rotator cuffs and osteoarthritis. On the flip side, it’s also common for people with chronic pain to show no sign of any tissue damage or structural abnormalities at all.
As Melaine Thernstrom says in her extraordinary book, The Pain Chronicles:
“The relationship between pain and tissue damage can be compared to the relationship between love and sex: it may or may not exist.”
So if people can have tissue damage with no pain and pain with no tissue damage…. What does this mean?
What I’m learning is that pain isn’t as straightforward as I thought. Pain is complex, unique to the individual, and multi-factorial, which means that the extent to which we experience pain is affected by both biological factors (think tissue damage and inflammation) AND psychological and social factors (think beliefs, emotions and stress). This way of understanding pain is called the bio-psycho-social model.
This doesn’t mean that pain is ‘all in your head’ and it certainly doesn’t mean that the body is irrelevant in the treatment of pain. It just might not be as relevant as you expect.
In some cases, a focus on biomechanics is appropriate. For example, I have pain in my Achilles tendon due to tendinopathy. In this case, progressively loading the tendon with calf raises has been the main course of treatment for curbing the pain. Simple. Problem solved. But for chronic pain with minimal tissue damage (which I also experience) a truly integrated approach to pain is needed: one that addresses the biological, the psychological and the social.
In some cases, biomechanical interventions may be the least effective strategy to help a person in pain.
A great deal of research has been done on the relationship between postural alignment and pain, and the correlation between ‘bad’ postural habits and pain is astoundingly weak.
Here are just a few examples taken from Todd Hargrove’s excellent article on the subject of pain and biomechanics:
- “Teenagers with postural asymmetry, excessive thoracic curve and/or lumbar curve were no more likely to develop back pain in adulthood than peers with “better” posture (Dieck 1985).
- Pregnant women with larger increases in low back curve during pregnancy were no more likely to develop back pain (Franklin 1998).
- A review of ten studies found no correlation between thoracic kyphosis and shoulder pain. (But there was less shoulder ROM) (Barrett 2016).
- Teenagers with slumped forward head postures didn’t have more neck pain (although they were more depressed.) (Richards 2016).
- No association between low back pain and spondylolisthesis (a condition where a vertebra has slipped forward, and which is often corrected by fusion surgery) (Andrade 2015).”
With so much evidence to the contrary, why do so many of us still focus on ‘correcting’ postural habits to treat pain?
In addition to possibly being ineffective, I’ve noticed for myself that this approach can be actively harmful as it causes me to focus on what’s (supposedly) ‘wrong’ with my body.
Some days felt a lot like this….
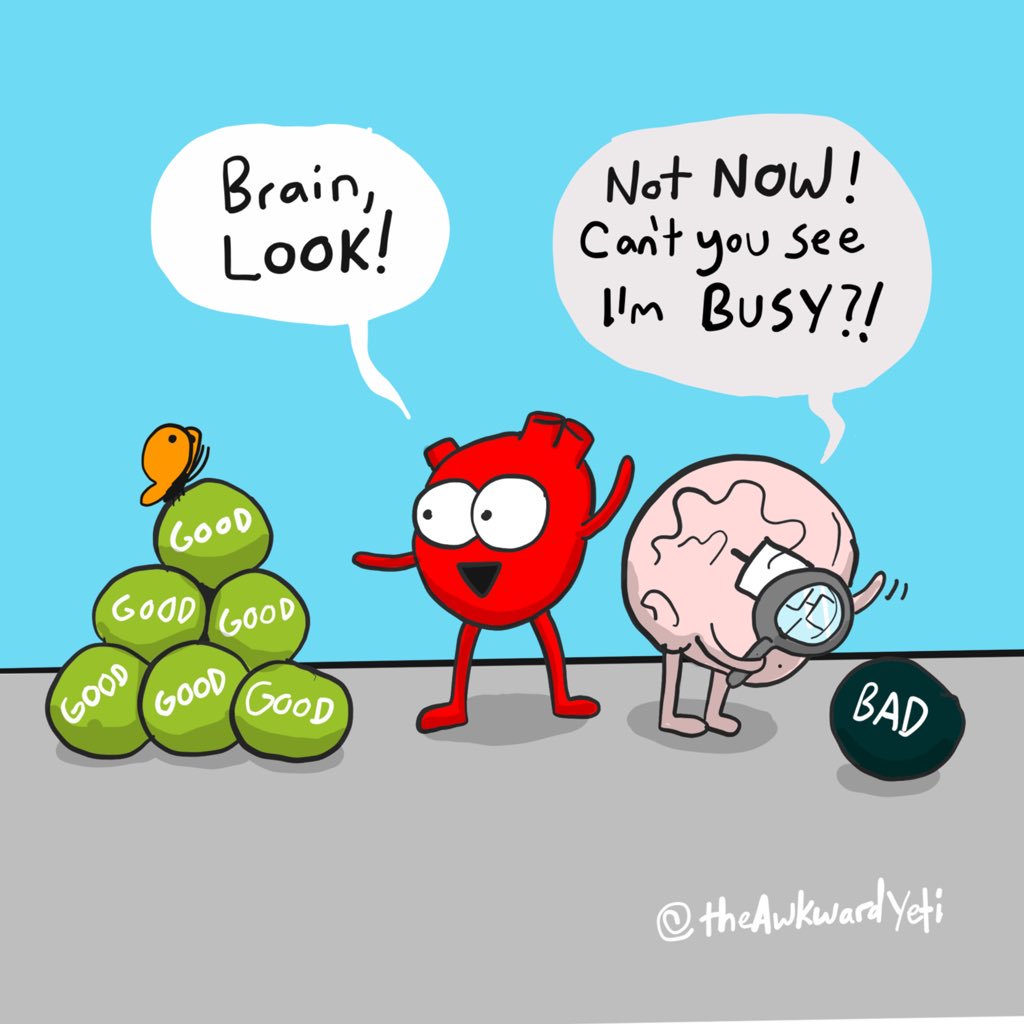
In fact, as I immersed myself in the world of pain science, I was astounded to realise just much fear and anxiety I was experiencing in relation to my pain.
I noticed that I wasn’t having much fun in my yoga and movement practices anymore because all my energy went to correcting my ‘defects’. In addition, I was convinced that something must terribly wrong in my tissues and I spent many hours in fearful contemplation of what that might be.
But now, feeling empowered by what I’m learning from pain science, I’m beginning to process and apply some pain science principles in my daily life.
I’m carefully reintroducing activities that I love – swimming, long walks, dancing, running, a more active yoga practice. And I’m exploring new ones, namely Feldenkrais, which I’ve found to be a wonderful way to safely explore fun, novel movements.
With the help of meditative practices like iRest Yoga Nidra, I’m examining my beliefs about my body. And I’m inviting in new concepts and possibilities: What if, instead of being weak, broken, and fragile, my body was actually resilient, adaptable, intelligent, and strong?
I’m not doing so many corrective exercises, I’m not searching for new health care practitioners in the hope that they will fix me (although I have found a pain specialist, whose help has been invaluable) and I’ve eased up on the freaking out and catastrophizing.
The result? My has pain eased significantly.
It’s not gone completely, and there definitely are some biomechanical factors at play which I’m working to address, but overall the level of physical, mental and emotional suffering I was experiencing has dramatically shifted in the direction of greater well-being. Instead of fear and frustration, I’m now much more likely to feel curiosity and awe towards this very human experience that we know so little about.
Although I’m still coming to grips with the implications of pain science, I find it to be a fundamentally hopeful and life-enhancing approach.
I know now that there are many things I can do to address my pain, of which biomechanics is just one. I feel hopeful that I can live a full and meaningful life, one in which I can move, play and feel good in my body. I even feel hopeful that I could do that alongside the experience of pain.
Pain just doesn’t seem so scary any more. Complex, mysterious, fascinating and strange, yes. Frustrating, often. But scary? Not anymore.
Recommended Pain Science Resources
- Recovery Strategies Pain Guidebook by Greg Lehman
- Interview with Greg Lehman on J. Brown Yoga Talks podcast
- Yoga and the New Science of Pain by Jenni Rawlings
- The Pain Chronicles: Cures, Myths, Mysteries, Prayers, Diaries, Brain Scans, Healing, and the Science of Suffering by Melanie Thernstrom
- Interview with Jules Mitchell on the Mindful Strength podcast
- PainScience.com
- Better Movement.com
Pain science is such an interesting topic!
I’m glad it’s helped you to stop focusing on the biomechanics and alignment. I guess we have a tendency to focus on those things because it makes us think we have the power to fix ourselves. When sometimes we really just need to let go of control and let our bodies fix themselves. Hmm.
The more I learn about the body and the mind, the more I realise that so many of the issues we have in our bodies are somehow linked to our mindset and mental state. And that by changing our mindset about something, we can sometimes alleviate the pain or discomfort in our bodies.
Thank you for sharing, this post definitely gave me something to think about. 🙂
Yes, it’s fascinating!
I’m glad this piece gave you some food for thought. I’m still learning, processing and contemplating these topics on a daily basis – I think it might be the work of a lifetime. Right now I’m really noticing how much the experience of pain varies for individuals – sometimes focusing on biomechanics can be very helpful, and sometimes not. Although it seems the general tendency is to focus on biomechanics, so it’s worth highlighting the other options available.
Thank you for your thoughtful comments,
Lucinda
That’s really interesting how it varies depending on the person!
I couldn’t agree more.
Camilla
Very helpful article! Stress is one of the key players when it comes to chronic pain and over thinking let it go to the next level. Thanks for sharing!
What medication is good for chronic pain, that one can function on?
Hi Shanaya,
I’m not an expert on pain medication. I suggest you find a pain specialist who can help you with this.
Wishing you all the best,
Lucinda
Excellent article Lucinda
Great article Lucinda – some awesome insights – thanks!